What is a Low Anterior Resection?
A Low Anterior Resection (LAR) involves surgical removal of a majority portion of, or the entire rectum and the sigmoid colon, while hooking up the remaining rectum with the end of the colon. This hookup is referred to as an "Anastomosis" and achieved during the LAR procedure by the colon and rectum being sewn or stapled back together. The goal of a LAR procedure is curative removal of a malignant rectal tumor.
Low anterior resections are usually used in treating stage II and III rectal tumors. LAR can also be used to treat upper, mid, and low rectal tumors – your surgeon will discuss with you and advise which procedure would best based on your unique situation and factors. LAR is generally performed for lesions in the middle and upper third of the rectum and, occasionally, for lesions in the lower third. Because this is a major operation, patients who undergo LAR should be in otherwise good health. They should not have any preexisting sphincter problems or evidence of extensive local disease in the pelvis.
A low anterior resection is done with general anesthesia, the patient is put into a deep sleep and doesn't feel pain. The surgeon makes several small incisions (cuts) in the abdomen. The cancer and a margin (edge or rim) of normal tissue around the cancer is removed, along with nearby lymph nodes and other tissues around the rectum.
The colon is then reattached to the remaining rectum so that a permanent colostomy is not needed. (A colostomy is needed when, instead of reconnecting the colon and rectum, the top end of the colon is attached to an opening made in the skin of the abdomen. Stool then comes out this opening.)
Note in images 1 and 2, how the initial anatomy can be loosely described as a 'question mark' (?) and how the potential future anatomy resembles a 'seven' (7). This difference in anatomy is important when considering the potential issues involved with LARS.
Image 1. Anatomy of the Colon & Rectum Prior to Low Anterior Resection
Image 2. Anatomy of the Colon & Rectum After Low Anterior Resection
Image 1 - The anatomy of the colon and rectum - highlighting a possible location in a Low Anterior Resection procedure.
Image 2 - Possible anatomy of the colon and rectum after Low Anterior Resection.
Note in images 1 and 2, how the initial anatomy can be loosely described as a 'question mark' (?) and how the potential future anatomy resembles a 'seven' (7). This difference in anatomy is important when considering the potential issues involved with LARS.
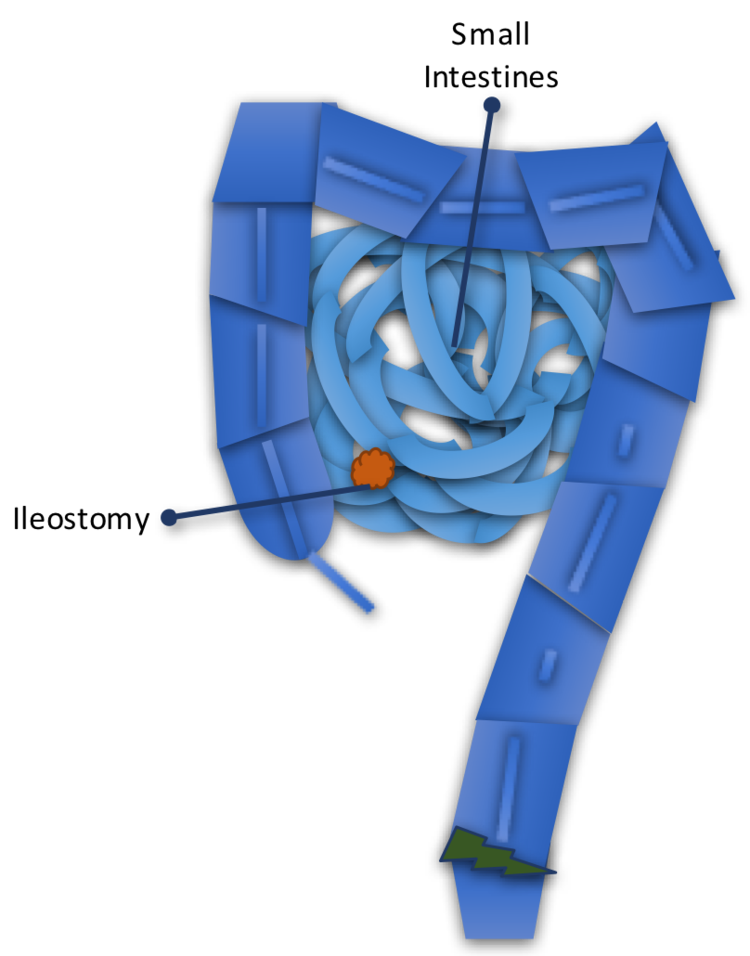
Loop Ileostomy
Following the LAR procedure, most rectal cancer patients undergo a Loop Ileostomy or Diverting Ileostomy. This ileostomy is usually temporary and diverts stool from the colon and resected rectum to allow for healing of the anastomosis, and instead the stool comes out of a stoma on the right side of the abdomen and into an ileostomy bag. [This is not to be confused with a colostomy, which is permanent and diverts into a stoma from the colon]
After a period of 4-6 months, the ileostomy is reversed, allowing stool to continue passing down into the colon and very quickly triggering the symptoms of LARS.
A key suspected factor causing LARS is this 4-6 month period of healing in the colon as the inactivity during this time can cause issues with stool motility among other factors, like colon flora.
Image 3. Anatomy of the Small Intestines with Loop Ileostomy Diverting from the Colon & Rectum after Low Anterior Resection
Image 3 - Loop Ileostomy is a temporary diversion of stool out of a stoma on the right side of your abdomen and into a ileostomy bag.
Medical Disclaimer - The information on this site is not intended or implied to be a substitute for professional medical advice, diagnosis or treatment. All content, including text, graphics, images and information, contained on or available through this web site is for general information purposes only. Love Your Buns makes no representation and assumes no responsibility for the accuracy of information contained on or available through this web site, and such information is subject to change without notice. You are encouraged to confirm any information obtained from or through this web site with other sources, and review all information regarding any medical condition or treatment with your physician. NEVER DISREGARD PROFESSIONAL MEDICAL ADVICE OR DELAY SEEKING MEDICAL TREATMENT BECAUSE OF SOMETHING YOU HAVE READ ON OR ACCESSED THROUGH THIS WEB SITE.
Love Your Buns does not recommend, endorse or make any representation about the efficacy, appropriateness or suitability of any specific tests, products, procedures, treatments, services, opinions, health care providers or other information that may be contained on or available through this web site. LOVE YOUR BUNS IS NOT RESPONSIBLE NOR LIABLE FOR ANY ADVICE, COURSE OF TREATMENT, DIAGNOSIS OR ANY OTHER INFORMATION, SERVICES OR PRODUCTS THAT YOU OBTAIN THROUGH THIS WEB SITE.